When reviewing medical software, we looked for features we considered central to the purpose of the platform. We considered these features absolute requirements for medical software platforms and paid close attention to how well each solution performed in our testing when it came to them. Below are some of the key features you should look for when choosing medical software.
HIPAA Compliance and Security Standards
All medical software must meet strict HIPAA compliance requirements to protect patient health information. According to the latest HHS guidance, new cybersecurity standards are being implemented in 2025 to strengthen protection of electronic protected health information (ePHI). Key requirements include:
- Administrative Safeguards: Every medical software platform must have designated security officers, workforce training programs, and documented security policies. Recent HIPAA updates require annual compliance audits and enhanced cybersecurity measures.
- Physical Safeguards: Medical software must ensure secure access to facilities and workstations where ePHI is accessed. This includes automatic logoff features, device controls, and secure disposal of electronic media containing patient data.
- Technical Safeguards: Current HIPAA-compliant software requirements include end-to-end encryption, access controls, audit logs, and secure data transmission protocols. All of our recommended platforms meet these stringent requirements.
- Business Associate Agreements: Any third-party software vendor that handles PHI must sign a Business Associate Agreement (BAA) with healthcare providers, ensuring they maintain the same security standards as the covered entity.
Appointment Scheduling
On the practice management side of medical software, appointment scheduling tools are fundamental to streamlining your front-office staff’s calendar-related tasks. Appointment scheduling features can also expedite intake and registration in ways not possible with traditional paperwork.
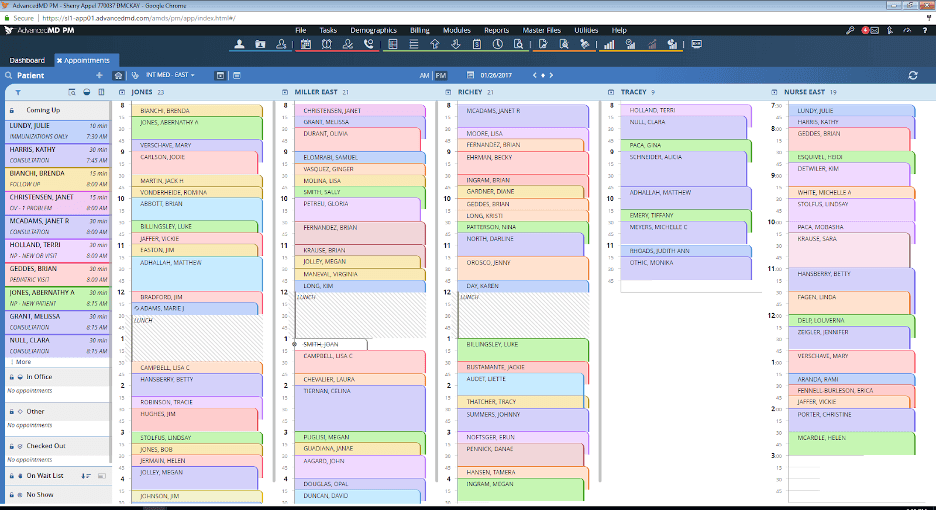
Although appointment scheduling is primarily a practice management software tool, you’ll also see it on the EMR side of most medical software platforms. Your medical software’s appointment scheduling tool should let you see your daily appointment schedule and appointment types. It should also display a patient’s status and location within your facility (or which facility they’re scheduled to visit). Some medical software allows you to track patients right down to the specific exam room or piece of medical equipment, as well as to check them out when their visit is complete.
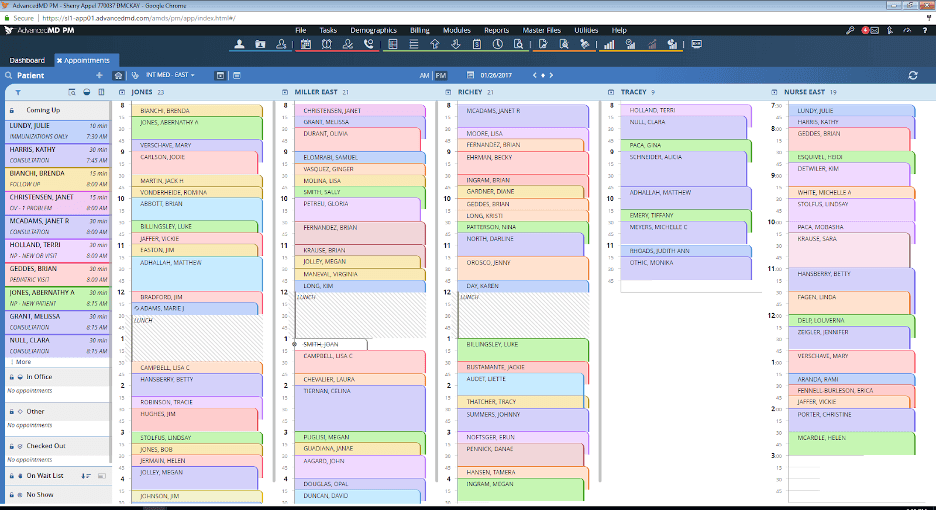
AdvancedMD allows customization of the appointment calendar, including color-coding appointment types so it’s easy to prepare for them at a glance. Source: AdvancedMD
Billing and Claims
The practice management software portion of your medical software tool should be able to post charges and create claims based on your EMR data. It should also have built-in ICD-10 and CPT coding libraries, alongside automatically generated E&M codes, that your billers can use.
The best medical software platforms should clearly indicate the patient and care provider tied to the claim, as well as the total claim value. Your software should also include claim-scrubbing tools, and many platforms have tools for handling rejected or denied claims too. Another critical function we looked for in our reviews is insurance eligibility verification. This allows you to check whether a patient’s insurance policy on file is active and up to date as soon as the appointment is scheduled. High-quality medical software enables you to check this information en masse.
Charting and Notetaking
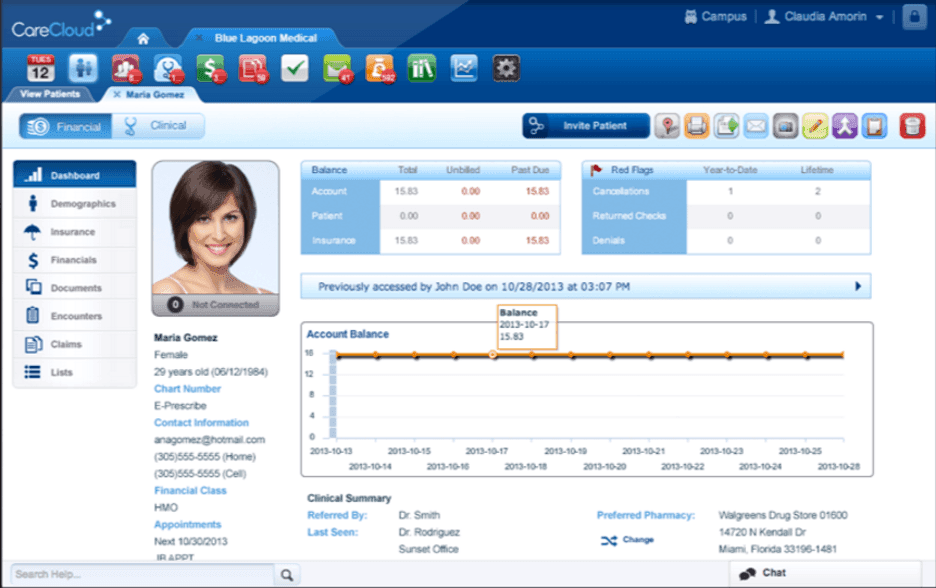
EMR software should make it easy to take notes during encounters and add information to patients’ charts, whether typing or using hotkeys or voice-to-text. Your patient charts should clearly show the patient’s vitals, current medications, recent appointment history, medical history and other basic information. They should also let you easily jump to other tools, such as your e-prescribing suite.
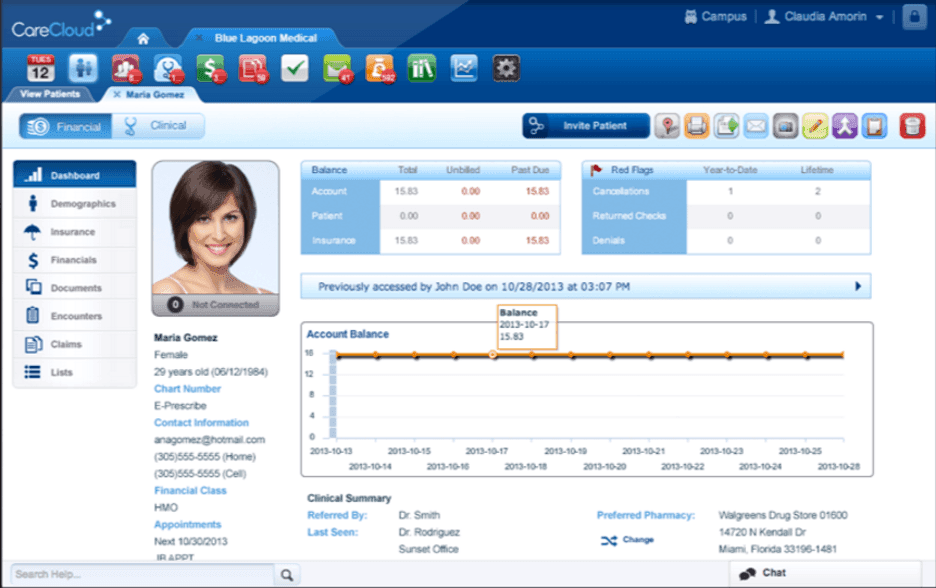
Medical software includes clinical tools such as patient charts. In the example above, a CareCloud patient chart displays basic patient information alongside a toolbar that can drill down further into their details. Source: CareCloud
Customization
In your EMR system, you should have access to numerous templates you can use to take notes during patient encounters or add important information to patient charts. Most importantly, these templates should be extensively customizable. You should be able to modify them based on the appointment type or your preferred notetaking method.
Your chosen template should give you a quick view of the most critical information for your encounter and fill in chart fields as needed. If a template isn’t working for you at the moment, some medical software platforms will let you tweak it as you take notes.
Medical software customization also extends to practice management software reporting. Many practice management software providers offer hundreds of customizable, filterable financial reports; in fact, we suggest not choosing platforms that offer little to no customization on the reporting side.
Customization is vital for both EMR and practice management software. Every healthcare organization has its own workflow, and your chosen medical software should be flexible enough to accommodate your practice’s unique needs and preferences.
E-Prescribing and Labs
Your medical software should make electronically prescribing medications a breeze. It should also give you the option to review a patient’s entire medication history. Most EMR platforms even flag potential drug interactions or medicines that could trigger a patient’s allergies.
Several medical software solutions also include tools for electronically ordering labs and bloodwork. These platforms typically integrate with leading lab providers such as Labcorp and Quest Diagnostics, though some of our best picks lack this capability. These standout products make up for this gap with the vast majority of their other features.
Interoperability
No two medical practices use precisely the same software suite, but practitioners often need to communicate with one another. Interoperability features ensure no information gets lost or misinterpreted in transmission between disparate systems. They also allow instant provider access to a patient’s medical data.
Interoperability is also fundamental to getting your practice’s vaccine and immunization data into the CDC’s immunization information systems. The Medicare and Medicaid EHR Incentive Programs also have several meaningful use standards that practices can and should achieve through interoperability measures.
Patient Portal
Many medical software companies include a patient portal with their practice management software offerings to expedite patients’ ability to book and modify appointments. Through these portals, patients can also request medication refills or message your front-office staff for assistance. Similarly, your front-office staff can use this portal to send patients their registration and intake forms, billing statements and payment requests.
Performance Management and Reporting
The best medical software includes customizable reports that can help you view and analyze all kinds of performance data tied to your practice’s operations. You can filter your reports based on numerous categories, such as provider, payer or location. With most platforms, you can also modify the period over which the information is collected and export your reports in several file formats.
Telehealth
As telehealth becomes increasingly important in modern healthcare, the best medical software includes plenty of telemedicine tools. Ideally, your chosen telehealth platform will fully integrate with your EMR system and practice management software for easy note taking and scheduling. In some cases, patients won’t have to download separate apps to start telehealth calls from their phones. This convenience may be useful to keep in mind as you browse medical software options.
If you’re looking for improved communications tools for your medical practice, we’ve also reviewed the
best business phone systems for medical offices. Check out our best picks to learn more about which phone systems stand out in the healthcare space.
Specialty-Specific Considerations
Medical software requirements vary significantly by specialty. Here are some examples of what certain specialists may need in their medical software:
- Dermatology: Requires image annotation capabilities, before/after photo storage, and procedure-specific templates for cosmetic and medical dermatology.
- Cardiology: Needs integration with ECG devices, ECHO systems, and specialized cardiac imaging tools. Cardiology-specific EMRs often include cardiac risk calculators and procedure templates.
- Orthopedics: Requires integration with radiology systems (PACS), procedure planning tools, and templates for musculoskeletal conditions and surgical planning.
- Mental Health: Needs specialized assessment tools, treatment plan templates, and compliance features for behavioral health documentation requirements.
All of our recommended general practice platforms offer some level of specialty customization, with AdvancedMD and athenahealth providing the most comprehensive specialty-specific features.